New perk: Easily find new routes and hidden gems, upcoming running events, and more near you. Your weekly Local Running Newsletter has everything you need to lace up! Subscribe today.
The Achilles tendon is the largest and strongest tendon in the human body and may be the most important tendon in the foot or leg for an athlete. One study found that acute and chronic Achilles tendon pathology is estimated to be responsible for as much as 50% of all sports-related injuries.
The injury is most commonly due to overuse or a sudden increase in training and activity. Note that there is no evidence in the medical literature that tightness of the Achilles leads to injury.
It’s important to point out that the proper terminology for Achilles problems is tendinopathy, not tendinitis. Studies have shown that the inflammatory period of an injury (which “-itis” indicates) is roughly over after 2 weeks, at which time the tendon injury changes to more a degenerative process—meaning tendinosis is the better terminology. This has implications for how the injury is treated.
The Achilles has several unique characteristics that set it apart from other tendons in the body. One is a poor blood supply to the area, which sometimes contributes to the chronic nature of Achilles injuries. If an injured tendon does not get adequate blood flow then healing becomes more difficult, since oxygen and healing factors are carried to the area by the blood vessels.

The anatomy of the tendon is unique, as it forms from 3 different muscles: the Medial and Lateral heads of the Gastrocnemius and the deeper Soleus muscle. The fibers also undergo a spiral rotation as the tendon leaves the muscle and attaches to the back of the heel bone (calcaneus). The tendon has a broad, thin attachment that spreads out over the entire back of the heel. Perhaps due to this uniqueness, there are 3 distinct areas that can become injured, leading to a forced rest or change in activity.
Finally, the Achilles functions via eccentric contractions, which means that the muscle-tendon complex is lengthening and firing at the same time. In contrast, during a concentric contraction the muscle-tendon is shortening and contracting simultaneously. Several muscles fire eccentrically at different times during the gait cycle, the main effect of which is to decelerate structures and help absorb impact and reduce forces through the leg.
Types of Achilles Tendinopathy
Achilles tendinopathy often starts insidiously, there may be some pain and stiffness one morning that goes away after you walk a few steps. This is the time to start treatment to prevent a longer forced rest.
My first rule for runners is that if you are limping then you should not be running! Like with a stress fracture, this is one injury where no running may be required. Please don’t view it only as a negative, take the time to improve your overall strength, flexibility and proprioception.
The most common type of injury to the tendon is midsubstance tendinopathy of the Achilles. This affects the area between the back of the heel and the end point of the 3 calf muscles (known as the Gatroc-Soleus complex).

The second type of pathology is Paratendinosis. The Achilles is surrounded by a special sheath known as the paratenon, a paper-thin covering that can sometimes develop scar tissue and lead to pain in the Achilles.
Sometimes it can be difficult to distinguish between midsubstance teninopathy and paratendinosis. One way to tell the difference is that the midsubstance tendinopathy of the Achilles hurts more at the start of the run and then warms up with less pain. The paratendinosis, however, may cause increased pain as the run progresses.
The final type of Achilles tendon pathology is insertional tendinopathy, which affects the connection point between the tendon and the heel bone.
Midsubtance Achilles Tendinopathy
When this injury becomes more advanced, swelling of the tendon may be noticeable. It is not really swelling, however, but rather a sign of thickening of the tendon from the start of the degenerative process. Once there is noticeable swelling you must stop running; if there is pain when running, you will compensate and sometimes that can lead a worse injury of a different part of the body. Cross train with non-impact activities such as pool running, swimming or the ElliptiGo.

The initial treatment plan should include rest, ice (apply at the end of the day for 15 minutes), taping, and gentle stretching. Note, however, that stretching and rest alone are not going to help get this tendon better and prevent further problems. Strengthening of the tendon and making sure the gluteal muscles are engaged are the best areas to focus on once the tendon initiates the degenerative process.
Eccentric Strength Training
To strengthen the tendon, Swedish orthopaedic surgeon and professor Håkon Alfredson developed an eccentric training program that has been proven to help resolve midsubstance Achilles Tendinopathy.
I have modified the protocol to perform the exercises on flat ground instead of off a step, as the step method leads to a negative heal drop which has led to some of my patients developing other injuries including tendinopathy of the Peroneal tendons, which run behind the lateral ankle bone.
If you have pain when doing a single leg-raise up off the heel, then start Achilles rehab by doing heel raises with both feet. Rise up off the heel, hold for a count of 2 and slowly lower down. Repeat the exercise, building up to 20 repetitions and stop if there is more than a little discomfort. Once you can progress to doing 20 with no pain, then you can change to a single-leg eccentric exercise: Go up off both heels, lift one foot in the air and slowly lower down on one side. Build up to 20 repetitions.
It is also important to address the glutes and make sure they are engaged and firing at the proper time. One aspect of modern society that has a negative impact on our bodies is the amount of sitting we do, which turns off the gluteal muscles. The Gluteus Minimus and Gluteus Medius are two of the most important core muscles for runners, and when they aren’t working properly, other structures, like the Achilles tendon, have to take on extra load that they are ill-suited to handle.
Here are 3 theraband exercises that work very well for the glutes. These exercises can be performed every day and I recommend doing them in a circuit. The first 10 days do one set of the full 3-exercise circuit. Then progress to doing each exercise twice, only if you can perform one set without much difficulty.
1. Clam Shells with Resistance
Start with 10 and build to 20 on each side.
2. Standing 4-Way Hip Pulls
Do 10–20 reps in each direction.
3. Butterfly Bridges
Start with 10 and build up to 20.
Another consideration with midsubstance Achilles injuries is to consider the drop of your shoes; this injury may respond better in a higher drop shoe. If you are in a zero drop shoe then perhaps consider trying a 4mm drop or higher for a short time to minimize the stress on the Achilles tendon.
If your injury progresses to the point of going to a sports medicine professional, extracoporeal shockwave therapy (ESWT) has been proven an excellent way to treat any type of Achilles tendinosis. There is more proof in the medical literature that ESWT works very well for Achilles tendon pathology as compared to treatments such as PRP (Platelet Rich Plasma) or Amniotic or Stem Cell injection.
Insertional Achilles Tendinosis
If you have problems at the point where the Achilles attached to the heel, forget everything that was written about midsubstance Achilles tendinosis—because insertional is completely different. Some treatments used for midsubstance, such as the eccentric heel raises, can make the pain worse for insertional. Runners with insertional achilles tendinosis often have bone spurring in the back of the heel bone.
One of the first and simplest treatments is to relieve pressure on the injured area. Most running shoes have a hard plastic piece in the back of the shoe known as the heel counter and often this will be the cause of painful insertional achilles tendinopathy. Try to find a shoe that works for you that does not have a heel counter. Several shoe companies offer options.

If you are unable to find a shoe without a heel counter that works for your stride and foot shape, then cutting out the back of the shoe can work well.

Icing, gentle stretching (should be felt in the calf, not at the insertion) and topical anti-inflammatories can work also well. A doctor can also prescribe the effective Flector patch, which is placed over the area for 12 hours and the anti-inflammatory will slowly be disseminated into the area. Surgery is sometimes necessary if conservative treatment fails but should be approached cautiously.
Achilles Paratendinosis
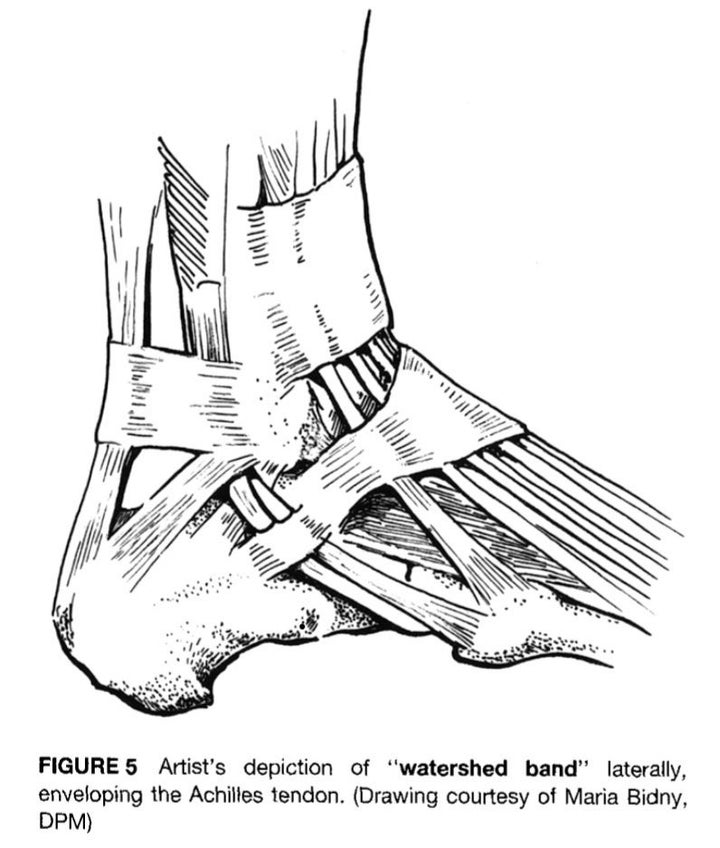
If the pain in the achilles increases as the run progresses then it could possibly be the paratenon that is the source. There is an organized area of the paratenon that often becomes thickened, known as the “Watershed band.”
Massage, icing and shockwave therapy are the best option for treatment of this injury. Eccentrics may not be much help. However, surgery to release the paratenon in cases that do not respond to conservative treatment has a high success rate with little down time compared to most other surgeries.
Be Early, Be Aggressive
If you have pain and swelling in the Achilles tendon be aggressive with your treatment. It is better to take time off and get it treated as soon as possible than to try and train through it. This is one time where no pain, no gain can be disastrous. The length of time to return to activity goes up the longer it takes for proper treatment to be started.
Dr. Brian Fullem practices at Elite Sports Podiatry, based in Clearwater, FL. He is a Fellow of the American Academy of Podiatric Sports Medicine. His is the author of The Runners Guide to Healthy Feet and Ankles.